
Overview of cows’ milk protein allergy in infants
Cows’ milk protein allergy (CMPA) is one of the most common food allergies in infants.1
Symptoms of CMPA include :
- Gastrointestinal (32-60% cases)
- Skin (5-90%)
- Anaphylaxis (0.8-9%)
- Respiratory
Many of these symptoms overlap. CMPA can be classified into two groups: IgE mediated or non-IgE mediated (delayed hypersensitivity).1 IgE mediated CMPA has a rapid onset of symptoms within minutes to an hour and can be diagnosed using tests such as skin prick tests or IgE bloods.2,3 Non-IgE mediated CMPA has a delayed onset and has negative results for IgE mediated testing and is usually diagnosed using food elimination and response to a hydrolysed formula.1,2,4 In gastro-oesophageal reflux (GORD) cases, 40% of infants may have underlying CMPA.5
Patient background
Patient X, a 4 month old term baby boy, was seen at the general paediatric clinic by the paediatric dietitian. The patient was referred for dietetic assessment regarding possible CMPA.
Patient X was exclusively breastfed for 4 days in hospital, then changed to a standard infant formula at home (Mum’s choice). When changed to a standard formula the patient started to show symptoms of poor feed tolerance. The patient’s mother described the following symptoms:
- Back arching post feeds
- Discomfort at night
- Large vomits soaking the baby, resulting in multiple outfit changes
- Reflux symptoms
- Constipation i.e. hard pasty stool once a day that baby strains to pass
- Crying and appearing in pain post feeds
This resulted in the patient’s parents trying different formula over the following weeks. The patient was initially changed onto a comfort formula, as advised by their health visitor. In addition to this, the parents also tried on their own accord an anti-reflux and a hungry baby formula; neither improved symptoms.
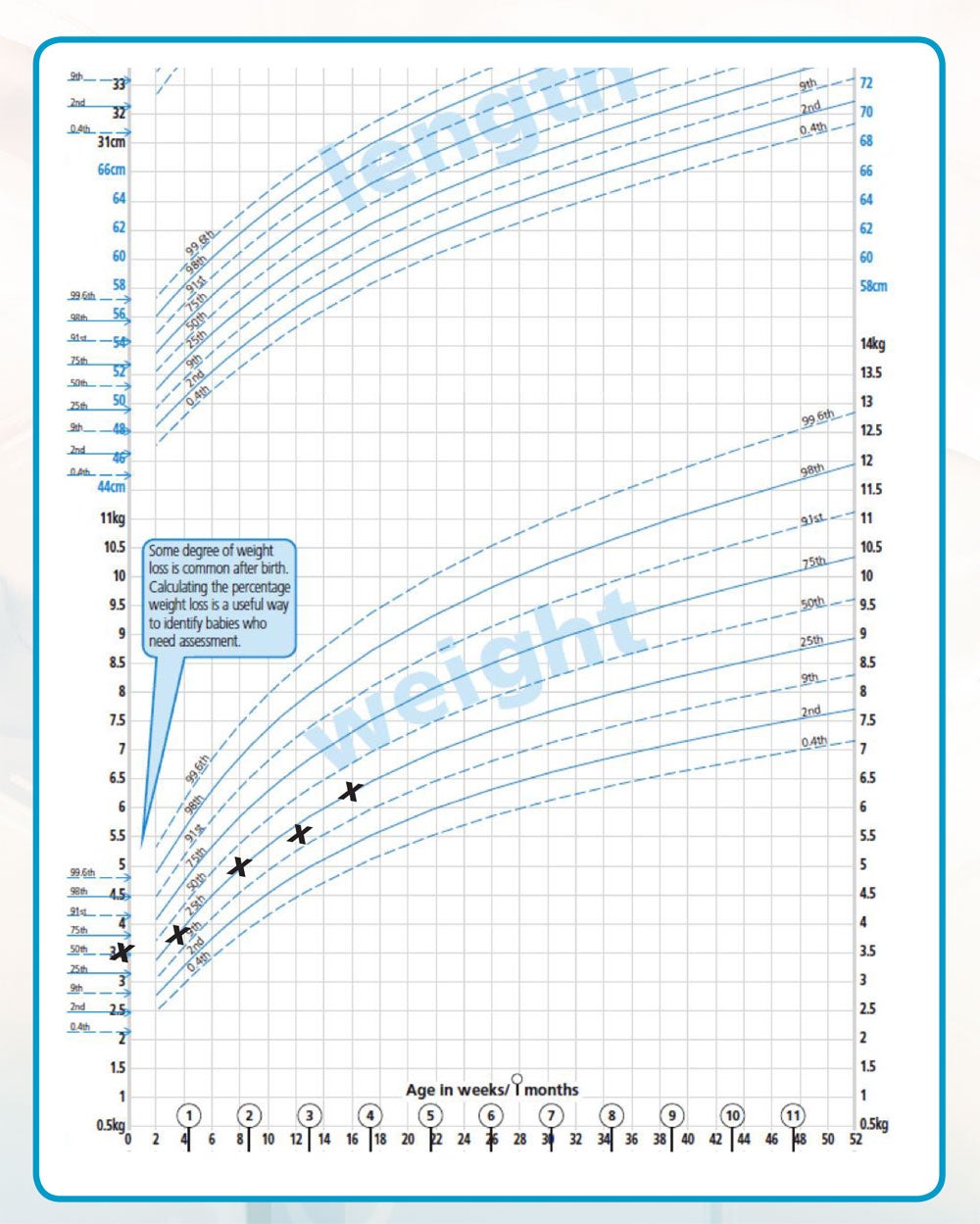
Despite the above symptoms the patient’s weight had continued to track the 25th centile as per the Red Book.
Medical history/interventions
The parents visited their GP who changed the patient’s formula to an extensively hydrolysed formula, as per the milk allergy in primary care (MAP) guidelines.4 The GP also referred the patient to the paediatric dietitian.
According to the mum, the patient was taking adequate volumes of feed: 160ml -180ml x 6 feeds per day (150ml/kg/day). He was also on Colief® Infant Drops (lactase enzyme), Gaviscon® Infant sachets (sodium alginate and magnesium alginate) and omeprazole (proton pump inhibitor – PPI); with some improvement in the reduction of frequent or large vomits. However symptoms including discomfort post feeds, crying and constipation persisted.
The paediatric dietitian initiated Neocate® LCP after the first consultation (the trust is currently under a Nutricia® contract). This amino acid based formula was chosen as symptoms were not fully resolved on the extensively hydrolysed casein formula (EHF), which is first recommended by the National Institute of Clinical Excellence clinical knowledge summary (NICE CKS) and the milk allergy in primary care (MAP) guidance when an infant has mild-moderate CMA symptoms.2,4 After two weeks the patient’s symptoms improved. The reflux resolved and the baby appeared more settled with reduced vomits. The stools also became softer.
However, due to the taste he was not taking adequate volumes of Neocate® LCP, so in desperation the parents changed back to an extensively hydrolysed formula on their own accord and his symptoms returned. The paediatric dietitian therefore decided to trial the infant on Alfamino®.
Medical and nutritional problems
GORD, constipation and CMPA were identified. In accordance with the MAP Guidelines4, the patient is likely to have non-IgE mediated CMPA.
Nutritional goals
- Control reflux symptoms using an amino acid based formula
- Ensure adequate volumes are consumed to support growth
- Adherance to a milk-free and soya-free diet until one year of age
- Challenge with cows’ milk at one year (it is the trust policy to challenge at one year of age)
Administration route/Volume administered
Oral
160ml -180ml x average 6 feeds per day (150ml/kg/day)
Reason for switching to Alfamino® (Nestlé Health Science)
Neocate® LCP was not accepted due to taste. To improve acceptability and volume intake the formula was switched to Alfamino® for its neutral taste.
Outcomes of feed change
Alfamino® (Nestlé Health Science) is a nutritionally complete amino acid based formula. Alfamino® was gradually increased by weaning off the extensively hydrolysed formula over a few days to promote acceptance of the new feed. The patient accepted Alfamino® and he began taking the same volume as before to meet his growth requirements. The patient continued on Alfamino® until one year of age and then cows’ milk was introduced using the MAP Milk Ladder according to tolerance.4
Discussion
CMPA is one of the most common cases of allergy seen in infants in my current practice. In this case there was a delay in being assessed by a paediatric dietitian as the patient was presented at 4 months of age. Fortunately the patient was still taking in enough calories to maintain adequate growth, despite the vomiting. CMPA infants should be seen promptly to resolve symptoms. This can in turn support growth and improve emotional well being by preventing feeding aversions, which can place a stress on both the parents and the baby,6 especially when the infant formula is not tolerated without any obvious reasons.
It is important to note that if a patient presents with CMPA, an EHF should be trialled and prescribed by their GP. A patient that does not improve on an EHF should be seen by a dietitian, to assess the suitability of an amino acid based formula.4
In addition to this they will receive milk-free feeding advice, weaning advice and the re-introduction of cows’ milk using the Milk Ladder at a later stage, usually after one year of age.4
The reasons for choosing Alfamino® besides its neutral taste, is that it is an amino acid based formula that is suitable for use in all cases of CMPA. It has a higher added medium chain triglyceride (MCT) content of 24.4% vs Neocate® LCP, which may help if fat malabsorption is present.7 It also has a low osmolarity of 300 mOsm/l which may result in better absorption of the formula and may reduce the risk of developing diarrhoea.8 It is also nutritionally complete from birth or supplementary feeding from 6 months up to 3 years of age. Additionally it is more cost effective feed when compared to other amino acid based infant formulas on the market.9
Summary
In summary, patient X presented with CMPA; he did not improve on an EHF. After trialling amino acid based formula Neocate® LCP, which was not accepted due to taste, the patient’s feed was changed to Alfamino®. There was a significant improvement in symptom resolution by switching to Alfamino®. The feed was also accepted due to its neutral taste. It is important to provide CMPA infants with a feed that not only resolves symptoms of CMPA, but is also accepted. This in turn promotes normal growth and development, but also provides parents with the assurance that their baby can feed normally.
Growth Chart
References
- Fiocchi A, Brozek J, Schünemann H et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. World Allergy Organ J 2010;3(4):57-161.
- NICE (2015) Clinical Knowledge Summary: Cow’s milk protein allergy in children: http:// cks. nice.org.uk/cows-milk-protein-allergy-in-children.
- Santos A, Dias A, Pinheiro JA. Predictive factors for the persistence of cow’s milk allergy. Pediatr Allergy Immunol 2010;21:1127-34.
- Venter C, Brown T, Shah N, Walsh J, Fox AT. Diagnosis and management of non-IgE-mediated cow’s milk allergy in infancy – a UK primary care practical guide. Clin Transl Allergy 2013;3(1):23. Available at: HYPERLINK “http://www.ctajournal.com/content/3/1/23”http:// www.ctajournal.com/content/3/1/23.
- Salvatore S, Vandenplas Y. Gastroeophageal reflux and cow milk allergy; is there a link? Pediatrics 2002; 110; 972-84.
- Lozinsky, A.C.; Meyer, R.; Anagnostou, K.; Dziubak, R.; Reeve, K.; Godwin, H.; Fox, A.T.; Shah, N. Cow’s Milk Protein Allergy from Diagnosis to Management: A Very Different Journey for General Practitioners and Parents. Children 2015, 2, 317-329.
- Marten B, Pfeuffer M, and Schrezenmeir J. Medium-chain triglycerides. International Dairy Journal 16: 1374-1382, 2006.
- Shaw, V & Lawson, M. (2007) Nutritional assessment, dietary requirements, feed supplementation. In Clinical Paediatric Dietetics, 3rd edn. eds V. Shaw & M. Lawson, pp 3-20. Oxford: Blackwell Publishing.
- MIMs September 2016.
IMPORTANT NOTICE: Mothers should be encouraged to continue breastfeeding even when their infants have cows’ milk protein allergy. This usually requires qualified dietary counselling to completely exclude all sources of cows’ milk protein from the mothers’ diet. If a decision to use a special formula intended for infants is taken, it is important to give instructions on correct preparation methods, emphasising that unboiled water, unsterilised bottles or incorrect dilution can all lead to illness. Formula for special medical purposes intended for infants must be used under medical supervision.
" MANAGING COWS’ MILK PROTEIN ALLERGY WITH ALFAMINO® Overview of cows’ milk protein allergy in infants Cows’ milk protein allergy (CMPA) is one of the most common food allergies in infants.1 Symptoms of CMPA include : Gastrointestinal (32-60% cases) Skin (5-90%) Anaphylaxis (0.8-9%) Respiratory Many of these symptoms overlap. CMPA can be classified into two groups: IgE mediated or non-IgE mediated (delayed hypersensitiv..."












